
Introduction to Medium-End Medical Equipment
Medium-end medical equipment occupies a pivotal role in the landscape of contemporary healthcare, bridging the gap between high-end, specialized apparatus and basic, essential tools. This category of medical devices is tailored to meet the needs of various healthcare facilities, such as hospitals and clinics, which require reliable and effective solutions without the exorbitant costs often associated with premium equipment. By enabling healthcare practitioners to deliver quality care, medium-end medical equipment enhances patient outcomes and operational efficiency.
The importance of this type of equipment cannot be overstated, particularly in settings where budget constraints are a reality. For many healthcare providers, medium-end medical equipment offers a viable and pragmatic choice, delivering essential functionalities while ensuring that investment costs are manageable. As healthcare technology continues to advance, medium-end devices have increasingly incorporated innovative features, maintaining a balance between cost and performance.
This comprehensive overview will delve into various categories of medium-end medical equipment, including diagnostic imaging devices, patient monitoring systems, laboratory instruments, and surgical tools. Each of these categories plays a significant role in the healthcare process, facilitating accurate diagnosis, effective treatment, and ongoing patient care. The integration of medium-end devices allows for greater accessibility to vital healthcare technologies, making them essential tools in the provision of quality medical services.
Throughout this exploration, specific examples and characteristics of the equipment will be discussed, allowing healthcare professionals to better understand the valuable contributions of medium-end medical equipment in their respective fields. The findings aim to underscore the importance and relevance of these devices as integral components of health systems, ensuring they continue to meet the evolving demands of patient care in an ever-changing healthcare environment.
ICU Monitoring Systems
ICU monitoring systems play an indispensable role in modern healthcare, particularly within intensive care units (ICUs), where they are crucial for real-time patient monitoring. These sophisticated systems are designed to track a multitude of vital signs and physiological parameters, including heart rate, blood pressure, respiratory rate, and oxygen saturation. By continuously collecting and displaying this vital information, ICU monitoring systems empower healthcare professionals to make informed decisions regarding patient care, especially for those who are critically ill.
The functionality of these monitors revolves around their ability to provide continuous surveillance of patients, alerting medical staff to any abnormalities that may arise. With advanced algorithms and data analysis capabilities, ICU monitoring systems present a comprehensive overview of a patient’s condition. This enables healthcare providers to quickly identify potential complications and respond proactively, which can be lifesaving in high-stakes environments such as the ICU.
In addition to basic vital sign monitoring, these systems often include advanced features such as trend analysis and alarm systems. Trend analysis allows healthcare professionals to view historical data and make predictions regarding a patient’s pathophysiological status. Alarm systems, on the other hand, ensure immediate attention is drawn to critical changes in a patient’s condition, facilitating timely interventions that can drastically improve outcomes.
Furthermore, ICU monitoring systems contribute significantly to enhancing interprofessional communication within the healthcare team. By providing a centralized platform where data from multiple devices can be displayed simultaneously, these systems foster collaboration among specialists, nurses, and support staff. Consequently, ICU monitoring systems not only enhance individual patient care but also streamline overall unit operations, proving to be invaluable assets in the management of critically ill patients.
Telemetry Systems
Telemetry systems have become an integral part of modern healthcare, allowing for the wireless transmission of patient data to healthcare providers. These advanced systems enable the continuous monitoring of vital signs, such as heart rate, blood pressure, and oxygen saturation, facilitating timely interventions while reducing the need for constant physical monitoring by healthcare professionals. By utilizing telemetry, data is collected and sent in real-time, promoting a proactive approach to patient care.
One of the most significant benefits of telemetry systems is their ability to enhance patient monitoring, especially in critical care settings. With access to real-time data, healthcare providers can make informed decisions swiftly, which is crucial during emergency situations. This immediate availability of patient information allows for quicker assessments and interventions, leading to better patient outcomes and reduced morbidity rates.
Furthermore, telemetry can significantly improve response times during emergencies. For example, if a patient’s vital signs exhibit concerning trends, the telemetry system raises alarms or alerts, ensuring that medical staff can respond almost instantaneously. This proactive monitoring capability not only augments patient safety but also optimizes resource management within healthcare facilities. Telemetry systems can be particularly advantageous in telehealth, where providers can monitor patients remotely, allowing individuals to receive care from the comfort of their homes without compromising safety.
In addition to immediate clinical benefits, these systems also enhance operational efficiency within healthcare institutions. By reducing the need for constant patient bedside presence, healthcare providers are empowered to allocate their time more effectively, focusing on more complex cases or providing necessary support to other patients. Overall, telemetry systems exemplify a significant stride towards improving patient care through enhanced data accessibility and real-time monitoring, making them an invaluable asset in the realm of healthcare technology.
Life Support Systems
Life support systems are vital components in patient care within healthcare settings, particularly in critical and emergency situations. These sophisticated devices are designed to sustain life by providing essential physiological functions that may be failing or compromised. The main types of life support systems include ventilators, cardiac monitors, and renal replacement therapies, among others. Each system plays a pivotal role in monitoring and supporting various life functions, ensuring that patients receive adequate care in life-threatening scenarios.
Ventilators, for instance, assist patients who are unable to breathe on their own by providing mechanical ventilation. They deliver oxygen-rich air to the lungs while removing carbon dioxide, thus facilitating gas exchange. Monitors continuously assess vital signs such as heart rate, blood pressure, and oxygen saturation, alerting healthcare personnel to any changes that may necessitate immediate intervention. Renal replacement therapies, including dialysis, perform the critical function of filtering waste and excess fluids from the blood, mimicking the natural processes of healthy kidneys.
To maximize the effectiveness of life support systems, integration with other medical technologies is crucial. For instance, electronic health record systems enable seamless communication among devices, providing a comprehensive view of patient data. This integration enhances decision-making, enabling healthcare professionals to respond more swiftly to patients’ needs. Additionally, these life-sensitive devices often rely on trained personnel, including doctors, nurses, and respiratory therapists, who possess the expertise to operate them correctly. The proficiency of these professionals is essential, as improper use of life support systems can lead to severe complications or even patient fatalities.
In essence, life support systems epitomize the intersection of technology and medicine, exemplifying how advanced devices can sustain life and enhance patient outcomes in critical healthcare scenarios.
Therapeutic Systems in Healthcare
Therapeutic systems play a critical role in modern patient care, being integral components of various medical treatments and processes. These systems encompass an array of therapeutic devices designed to alleviate symptoms, assist in recovery, and enhance the quality of life for patients suffering from various acute and chronic conditions. Among the notable types of therapeutic devices are those used in respiratory therapy and renal replacement therapy.
Respiratory therapy systems include mechanical ventilators, nebulizers, and CPAP (Continuous Positive Airway Pressure) machines. Mechanical ventilators are essential for patients who are unable to breathe adequately on their own, providing necessary ventilation support. They are often utilized in critical care settings, particularly in patients affected by conditions such as acute respiratory distress syndrome (ARDS) or chronic obstructive pulmonary disease (COPD). Nebulizers allow for the administration of aerosolized medications directly to the lungs, facilitating effective treatment of respiratory conditions like asthma and bronchitis. CPAP devices are utilized primarily in the management of obstructive sleep apnea, helping maintain an open airway during sleep, thereby improving overall health outcomes.
On the other hand, renal replacement therapy is vital for patients suffering from end-stage renal disease. This system consists mainly of dialysis machines, which perform the critical function of filtering waste and excess fluids from the blood when the kidneys can no longer fulfill this task effectively. Hemodialysis and peritoneal dialysis are the principal forms of renal replacement therapy, each catering to different patient needs and preferences. These therapies are crucial for maintaining metabolic balance and preventing complications associated with kidney failure.
In summary, therapeutic systems are pivotal in managing chronic diseases and facilitating recovery processes. With advancements in technology and continuous development in therapeutic device efficacy, these systems are better equipped to enhance patient care and promote positive health outcomes.
Nurse Call Systems
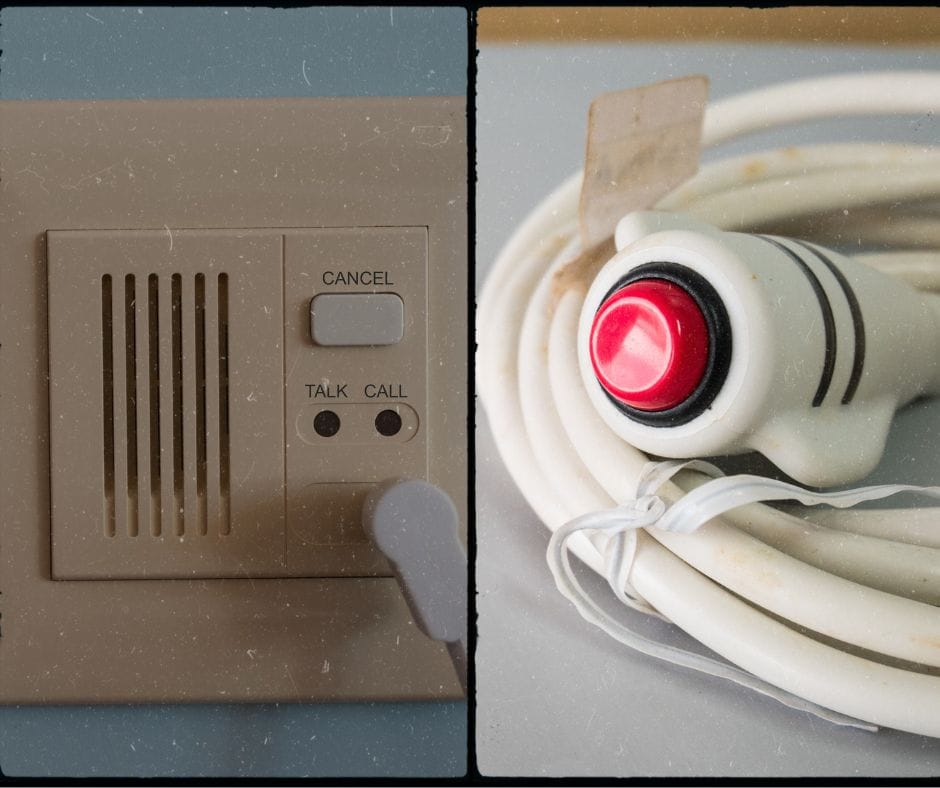
Nurse call systems have become an integral component of healthcare environments, significantly improving communication between patients and healthcare providers. These systems serve as a critical link, enabling patients to request assistance with ease and ensuring that healthcare providers can respond promptly. The operational essence of these systems lies in their capacity to facilitate communication—when a patient activates a call button, a signal is dispatched to nursing staff, thereby enhancing responsiveness in patient care.
The role of nurse call systems extends beyond mere communication; they play a vital part in improving patient satisfaction. By allowing patients to immediately alert staff to their needs, these systems help in enhancing the overall patient experience. Efficient nurse call systems reduce anxiety by providing patients with a sense of security and assurance that help is readily available. Additionally, when patients can communicate with their caregivers seamlessly, the likelihood of a positive healthcare interaction increases significantly, leading to higher satisfaction rates.
Technological advancements have drastically transformed nurse call systems, making them more user-friendly and efficient. Innovations such as mobile applications enable caregivers to receive alerts on their personal devices, allowing for quicker response times regardless of their location within the healthcare facility. Additionally, some modern systems incorporate advanced features such as video call capabilities and integration with electronic health records (EHRs), which enhance the user experience and streamline communication processes further.
As healthcare facilities continue to evolve, the importance of these systems cannot be overstated. They represent a foundational element of patient care, contributing to positive health outcomes and fostering an environment where effective communication is prioritized. As technology continues to improve, nurse call systems will likely become even more responsive and integral to the holistic approach of modern healthcare.
Infant Protection Systems
Infant protection systems play a crucial role in safeguarding newborns within healthcare institutions. The safety and security of infants in hospitals is of paramount importance, as new parents seek reassurance that their children are protected from potential threats. These systems are designed to prevent infant abduction and wandering, leveraging advanced technologies to ensure the well-being of patients and provide peace of mind to their families.
One of the primary technologies employed in infant protection systems is the use of electronic tagging. Each infant is secured with a small, tamper-proof bracelet that contains an embedded radio-frequency identification (RFID) chip. This chip allows for real-time monitoring of the infant’s location within the hospital premises. Should an attempt be made to remove the bracelet or move the infant outside designated areas, an alarm is triggered, alerting hospital staff immediately. This proactive approach significantly reduces the risk of abduction and enhances the overall security protocol.
In addition to RFID technology, many hospitals implement surveillance systems that include CCTV cameras strategically positioned throughout maternity and neonatal wards. These cameras work in tandem with alarm systems, providing a visual deterrent to hospital visitors. Meanwhile, nurses and security staff are trained to monitor unexpected activities and to respond swiftly to potential security breaches. The integration of personnel training with technological systems is essential for the efficacy of infant protection protocols.
Protocol adherence is another critical component of infant protection systems. Hospitals often establish comprehensive guidelines that dictate how personnel should manage infant security. These guidelines cover everything from admission and discharge processes to staff identification procedures and visitor management. Regularly scheduled staff training sessions are crucial for reinforcing these protocols, as they ensure that all team members are well-informed about the latest security measures and aware of their responsibilities. By combining technology and well-defined procedures, healthcare facilities can create a safe environment for infants and foster trust among families.
Infusion Systems
Infusion systems play a critical role in modern healthcare, serving as vital tools for the precise administration of medications and fluids to patients. These systems are designed to deliver controlled amounts of intravenous (IV) solutions, including medications, nutrients, and blood products, directly into a patient’s bloodstream. By ensuring accurate dosing, infusion systems help healthcare providers to manage complex treatment protocols effectively.
There are various types of infusion pumps utilized in hospitals, each tailored for specific applications. The most common classifications include volumetric infusion pumps, syringe pumps, and patient-controlled analgesia (PCA) pumps. Volumetric infusion pumps are typically used for larger volumes and allow for high precision in fluid delivery. Syringe pumps, on the other hand, are best suited for smaller volume infusions and are often employed in critical care settings. PCA pumps empower patients to self-administer pain relief, giving them more control over their treatment and improving overall satisfaction.
Advancements in infusion systems are markedly enhancing patient care and safety. Features like smart infusion technology integrate software that helps to reduce medication errors, ensuring that the correct drug is delivered at the right dosage and rate. These systems often incorporate alerts for potential adverse drug interactions or miscalculations, which can significantly improve treatment outcomes. Moreover, wireless communication capabilities allow for real-time monitoring of patient data, facilitating immediate responses to any anomalies in infusion therapy.
As hospitals and healthcare providers continue to adopt advanced infusion systems, there is a promise of improved reliability, increased patient safety, and enhanced outcomes. Ongoing innovations in this field are essential to meet the demands of modern medicine and ensure that patients receive the highest quality of care during their treatment processes.
Radiology Information Systems (RIS) and Laboratory Information Systems (LIS)
Radiology Information Systems (RIS) and Laboratory Information Systems (LIS) serve critical roles in the healthcare environment, particularly in the management of patient data and operational efficiency. Both systems are designed to enhance workflow processes within their respective fields—radiology and laboratory services—yet they possess distinct functionalities tailored to their specific environments.
A RIS primarily focuses on the radiology department, aiming to manage imaging orders, patient scheduling, and report generation. Through the implementation of RIS, radiologists can access and share patient information swiftly, ensuring timely diagnosis and treatment. The integration of RIS with Picture Archiving and Communication Systems (PACS) further streamlines operations by allowing real-time image retrieval and sharing, thus significantly improving interdepartmental communication. This connectivity enhances collaboration between radiologists, referring physicians, and allied health professionals, ultimately elevating the standard of patient care.
Conversely, Laboratory Information Systems (LIS) manage laboratory operations, including specimen tracking, result reporting, and quality control processes. LIS systems are integral in ensuring that laboratory personnel can efficiently handle various samples and tests while maintaining accuracy in results. By automating workflows, LIS reduces the potential for human error, which is crucial in laboratory settings where precision is paramount. Additionally, LIS facilitates communication between laboratory staff and clinicians, providing crucial test results and insights that are essential for clinical decision-making.
While both RIS and LIS share common goals—enhancing workflow efficiency and improving patient outcomes—they operate in distinct contexts with specialized functions. By informing healthcare providers and enhancing operational capabilities, these systems contribute significantly to the effective functioning of radiology and laboratory departments, ultimately driving improvements in overall healthcare delivery.
Hospital Information Systems (HIS)
Hospital Information Systems (HIS) represent a crucial component in the modern healthcare landscape, serving as a pivotal tool for managing both administrative and clinical functions within healthcare facilities. HIS encompasses a range of software applications designed to facilitate the collection, storage, retrieval, and sharing of patient data, thus bridging the gap between healthcare professionals and the information they require for effective decision-making.
A primary feature of HIS is its ability to integrate various departmental functions within a hospital. This integration encompasses functionalities such as patient registration, scheduling, billing, and electronic medical records (EMR). By centralizing these operations, Hospital Information Systems enhance workflow efficiency, reduce redundancy, and minimize the potential for errors. For instance, the seamless communication enabled by HIS allows staff in different departments to access and update patient records in real time, fostering a collaborative environment that is essential for patient care.
Furthermore, HIS plays a pivotal role in enhancing decision-making processes. The system provides healthcare professionals with timely access to critical patient information, allowing for informed clinical decisions. Advanced data analytics capabilities enable hospitals to track performance metrics, forecast patient admissions, and manage resources more effectively. This data-driven approach not only supports improved operational efficiencies but also directly contributes to better patient outcomes by ensuring that clinicians have the most accurate information at their fingertips.
In addition to streamlining internal functions, HIS can improve patient care through enhanced data management. Effective data management promotes more personalized treatment approaches by analyzing patients’ historical data and predicting their healthcare needs. Overall, Hospital Information Systems streamline operations within healthcare facilities, enhance decision-making processes, and ultimately improve the quality of patient care.



 Healthcare
Healthcare